Children with cancer more likely to have severe COVID-19 illness

Children with cancer who contracted COVID-19 developed more serious infections and had a greater likelihood of hospitalization or death than the general pediatric population, according to study results published in The Lancet Oncology.
Moreover, data from the Global Registry of COVID-19 in Childhood Cancer suggest the severity of these children’s COVID-19 outcomes may be influenced by biologic and regional economic factors.
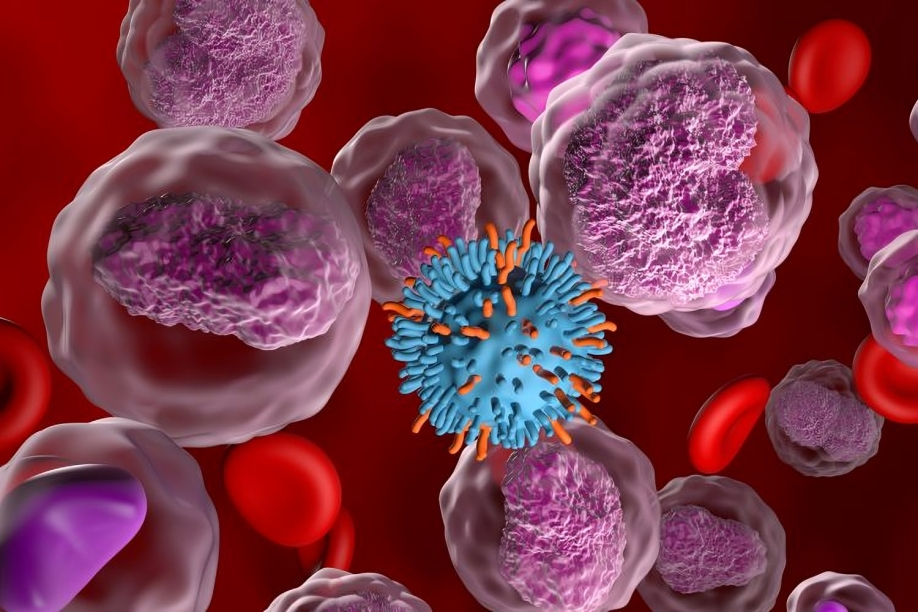
Children with cancer who contracted COVID-19.
Launched by St. Jude Children’s Research Hospital and the International Society of Pediatric Oncology, the registry collected data on the pandemic’s effect among the pediatric cancer population worldwide. The effects identified in the study appeared more pronounced in low- and middle-income countries, where children with cancer and COVID-19 have a sixfold greater likelihood of developing severe or critical disease compared with those in high-income countries.
Sheena Mukkada, MD
“The results clearly and definitively show that children with cancer fare worse with COVID-19 than children without cancer,” researcher Sheena Mukkada, MD, faculty member in the departments of global pediatric medicine and infectious disease at St. Jude, said in a press release. “This global collaboration helps clinicians make evidence-based decisions about prevention and treatment, which, unfortunately, remain relevant as the pandemic continues.”
Mukkada spoke with Healio about the study and what should be done to protect children with cancer who may be especially vulnerable to severe COVID-19 illness.
Study results
For the multinational cohort study, Mukkada and colleagues evaluated data from 131 institutions in 45 countries on laboratory-confirmed SARS-CoV-2 infections among children and adolescents aged younger than 19 years with cancer or history of a hematopoietic stem cell transplantation.
The study included 1,500 patients (median age, 8 years) between April 15, 2020, and Feb. 1, 2021, of whom 1,319 had full 30-day follow-up data available.
Disease severity and modification of cancer treatment regimens served as the primary outcomes.
Results showed 889 patients (67.4%) underwent hospitalization and 231 (17.5%) required admission or had to be transferred to a higher level of care.
In addition, 259 (19.9%) of 1,301 patients had infection that would be categorized as severe or critical, and 50 (3.8%) of 1,319 died due to COVID-19-related causes. In studies of the general pediatric population, only 1% to 6% reported severe COVID-19 infections, with mortality rates of 0.01% to 0.7%, according to the press release.
“Our study was not designed to capture the ‘why’ behind the poorer outcomes,” Mukkada told Healio, “but descriptively, we can see that those with lower numbers and function of immune cells, as well as those who were receiving more immunosuppressive therapy, have more severe disease.”
Among 1,092 patients undergoing active cancer treatment, 609 (55.8%) had modifications to their cancer-directed therapy and 44.6% had chemotherapy withheld during COVID-19 treatment.
Factors associated with higher likelihood of severe or critical illness on multivariable analysis included World Bank country income level (low-income or lower-middle income, OR = 5.8; 95% CI, 3.8-8.8; upper-middle income, OR = 1.6; 95% CI, 1.2-2.2); age 15 to 18 years (OR = 1.6; 95% CI, 1.1-2.2); absolute lymphocyte count of 300 or less cells per mm3 (OR = 2.5; 95% CI, 1.8-3.4) or 500 or less cells per mm3 (OR = 1.8; 95% CI, 1.3-2.4); and intensive treatment (OR = 1.8; 95% CI, 1.3-2.3).
Factors linked to treatment modifications included upper-middle income country status (OR = 0.5; 95% CI, 0.3-0.7), primary diagnosis of hematologic malignancies other than acute lymphoblastic leukemia or acute lymphoblastic lymphoma (OR = 0.5; 95% CI, 0.3-0.8); symptomatic COVID-19 at presentation (OR = 1.8; 95% CI, 1.3-2.4) and one or more comorbidities (OR = 1.6; 95% CI, 1.1-2.3).
Next steps
The study was conducted before vaccinations were available to older children in some areas of the world and before the identification of certain COVID-19 variants, including the delta variant. It is not clear whether these variables would affect the findings, Mukkada said.
“Vaccination is still not widely available in many of the places contributing to this study,” Mukkada told Healio. “We didn’t look at rates of transmission, just at what happened to infected patients, so it’s not clear that those findings would change due to vaccination.”
The registry offers insight into the potential risks for the pediatric cancer population, Mukkada said.
“The majority of children with cancer do not develop severe disease due to COVID-19,” she said. “However, disease can be severe in certain groups, so we must do what we can to protect this potentially vulnerable population, including optimal infection prevention and vaccination of qualifying patients and caregivers.”
References:
Mukkada S, et al. Lancet Oncol. 2021:doi:10.1016/S1470-2045(21)00454-X.
Press release. COVID-19 in children with cancer: Severe disease and disrupted treatment. Available at: COVID-19 in children with cancer: Severe disease and disrupted treatment – St. Jude Children’s Research Hospital (stjude.org). Accessed Aug. 31, 2021.